Exam Details
Exam Code
:USMLE-STEP-2Exam Name
:United States Medical Licensing Step 2Certification
:USMLE CertificationsVendor
:USMLETotal Questions
:738 Q&AsLast Updated
:Apr 12, 2025
USMLE USMLE Certifications USMLE-STEP-2 Questions & Answers
-
Question 661:
A63-year-old man with chronic bronchitis presents to the emergency department with worsening shortness of breath. He is dyspneic, his respiratory rate is 32/min, and he has peripheral cyanosis. A chest examination reveals increased anteroposterior diameter and scattered rhonchi, but no wheezes or evidence of consolidation. His ABG determinations on room air are pH of 7.36, arterial oxygen pressure (PaO2) of 40 mmHg, and PaCO2 of 47 mmHg. He is given oxygen by face mask while awaiting a CXR. His respiratory rate falls to 12/min,but his ABGs on oxygen are now pH of 7.31, PaO2 of 62 mmHg, and PaCO2 of 58 mmHg. Which of the following is the most appropriate next step in the management of this patient?
A. repeat the ABG
B. initiate mechanical ventilation
C. obtain a CXR
D. check the oxygen delivery system
E. decrease the fraction of inspired oxygen (FIO2)
-
Question 662:
A 23-year-old man presents complaining of severe crampy abdominal pain and blood in his stool over the past 2 days. Asimilar episode occurred a few months ago and spontaneously resolved. No history of travel. Abdominal x-ray shows mild colonic dilatation. Which of the following is the most likely diagnosis?
A. ulcerative colitis
B. viral gastroenteritis
C. irritable bowel syndrome
D. celiac sprue
E. Whipple disease
-
Question 663:
A60-year-old man presents with a nonproductive cough for a week and generalized malaise. He also has noted some abdominal pain associated with diarrhea for the past few days. His temperature is 101.5°F a nd clinical examination is unremarkable. ACXR shows a left lower lobe infiltrate. His urinalysis shows 50 RBCs, and his BUN (30) and creatinine (1.6) are both mildly elevated. In light of the extrapulmonary symptoms and signs, which of the following is the most likely cause of his pneumonia?
A. Pseudomonas aeruginosa
B. S. aureus
C. H. influenzae
D. S. pneumoniae
E. Legionella
-
Question 664:
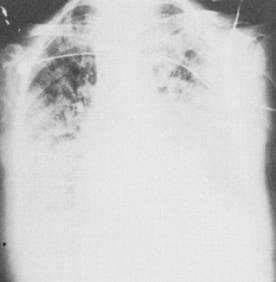
A 63-year-old man complains of a new cough and of breathlessness after walking up a flight of stairs. Chest examination reveals late inspiratory crackles but no wheezes. There is a mild clubbing of the fingers. His CXR is shown in figure. Which of the following would be found on pulmonary function testing (PFT)?
A. increased arterial carbon dioxide pressure (PaCO2)
B. normal compliance
C. decreased carbon monoxide diffusing capacity (DLCO)
D. increased vital capacity
E. increased oxygen saturation with exercise
-
Question 665:
A50-year-old woman complains of worsening dyspnea of 1-month duration, but is otherwise asymptomatic. Lung examination is normal; her CXR is shown in the figure below. Which of the following is the most likely diagnosis?

A. pulmonary tuberculosis
B. lung metastases
C. sarcoidosis
D. mycoplasma pneumonia
E. silicosis
-
Question 666:
In this otherwise healthy adult woman, what is the most likely infecting organism?
A. group B Streptococcus
B. Staphylococcus aureus
C. Haemophilus influenzae
D. Streptococcus pneumoniae
E. Listeria monocytogenes
-
Question 667:
In the adult neutropenic patient, which of the following is the most likely organism to cause bacterial meningitis?
A. group B Streptococcus
B. S. aureus
C. H. influenzae
D. S. pneumoniae
E. L. monocytogenes
-
Question 668:
A 78-year-old woman comes to your primary care office practice with her son who is concerned about changes in her mood. She is less interested in going out to dinner and does not want to visit family or friends. Her language skills seem to have deteriorated over the last few years and her memory is not as sharp. Her gait and motor strength are normal. Which of the following is the most likely diagnosis?
A. Parkinson's disease
B. anxiety disorder
C. meningioma
D. Alzheimer's disease
E. dysthymia
-
Question 669:
A44-year-old secretary presents with a fever of 103°F, headache, and stiff neck. You entertain a diagn osis of bacterial meningitis and begin antibiotics immediately. With bacterial meningitis, which of the following is a likely finding in the cerebrospinal fluid (CSF)?
A. leukocytes between 100 and 500/mm
B. CSF pressure between 100 and 120 mmH2O
C. negative Gram stain
D. glucose >120 mg/dL
E. protein levels >45 mg/dL
-
Question 670:
A42-year-old patient suffering from alcoholism has advanced liver disease with ascites. He is hospitalized for agitation and bizarre behavior. Which of the following findings is most helpful in making the diagnosis of hepatic encephalopathy?
In the patient above, his blood ammonia level is twice his baseline. Which of the following is a likely precipitating factor?
A. bleeding esophageal varices
B. noncompliance with diuretic therapy
C. excessive lactulose therapy
D. insufficient protein ingestion E. recent alcohol ingestion
Tips on How to Prepare for the Exams
Nowadays, the certification exams become more and more important and required by more and more enterprises when applying for a job. But how to prepare for the exam effectively? How to prepare for the exam in a short time with less efforts? How to get a ideal result and how to find the most reliable resources? Here on Vcedump.com, you will find all the answers. Vcedump.com provide not only USMLE exam questions, answers and explanations but also complete assistance on your exam preparation and certification application. If you are confused on your USMLE-STEP-2 exam preparations and USMLE certification application, do not hesitate to visit our Vcedump.com to find your solutions here.